Understanding MPOX: Symptoms, Treatment, and Prevention
Understanding MPOX: A Comprehensive Overview
MPOX, which stands for Monkeypox, is a viral disease that has garnered significant attention due to its emergence and transmission patterns. Initially discovered in 1958 in laboratory monkeys, the disease is now recognized as a zoonotic pathogen that can spread from animals to humans and has been noted for its clinical similarities to smallpox.
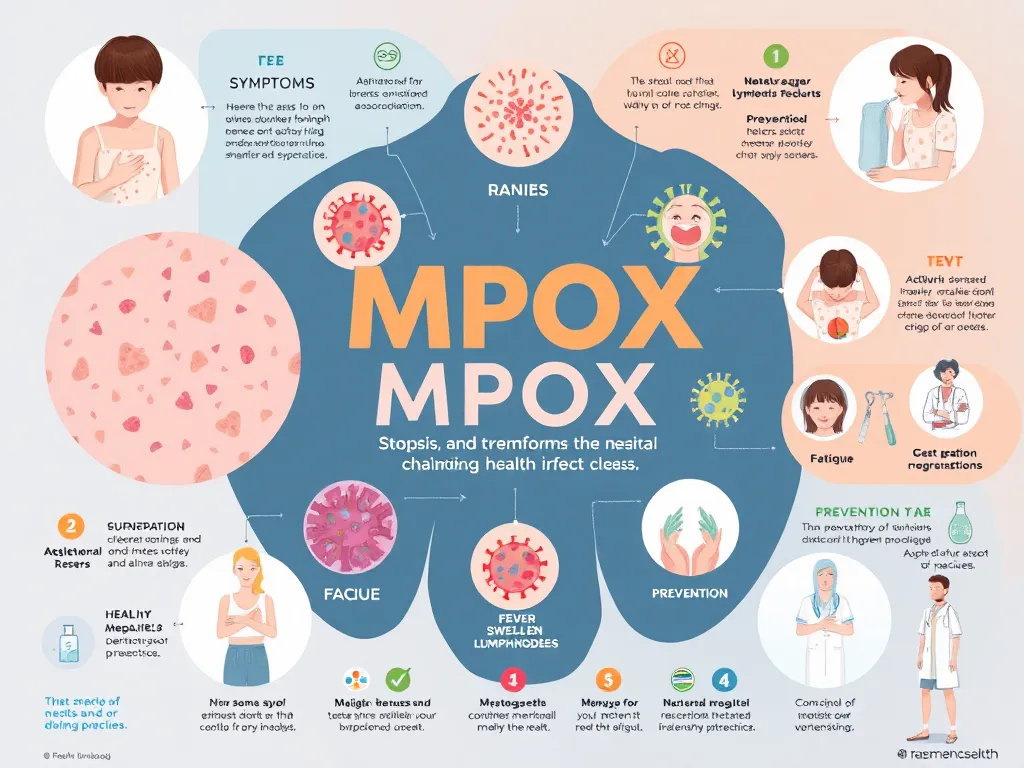
The virus responsible for MPOX is part of the Orthopoxvirus genus, which includes other pox viruses such as smallpox and cowpox. MPOX typically manifests with a series of flu-like symptoms followed by a rash that progresses to fluid-filled lesions. Exposure to infected animals or humans constitutes the primary mode of transmission, which has raised public health concerns, particularly in regions where the virus is endemic.
Symptoms of MPOX can take up to two weeks to appear after infection, and they often include fever, chills, headache, muscle aches, backache, swollen lymph nodes, and exhaustion. A notable aspect of MPOX infection is that the rash appears as fluid-filled blisters that can cause significant discomfort and may require medical attention.
MPOX has been increasingly observed outside of its endemic regions, with cases reported in multiple countries that were previously thought to be at low risk for the disease. The rise in worldwide cases, along with the potential for outbreaks in densely populated areas, has led to increased surveillance and research efforts to understand the epidemiology of MPOX.
As public health agencies explore ways to manage and contain MPOX outbreaks, the need for clear communication, vaccination strategies, and community support systems has become paramount. Understanding the behavior of the virus and its transmission dynamics will play a critical role in controlling future incidents of MPOX.
Symptoms of MPOX
Common signs of MPOX infection include a sudden onset of fever, fatigue, and swollen lymph nodes, followed by the development of a characteristic rash. The rash typically begins on the face and then spreads to other parts of the body, including the palms of the hands and soles of the feet. Lesions can be painful and lead to complications if they become infected with bacteria.
Differentiating MPOX from other viral infections such as chickenpox or smallpox can be challenging without laboratory testing. However, the presence of swollen lymph nodes and the order of lesion appearance are key indicators. Unlike chickenpox, which produces widespread lesions quickly, MPOX lesions tend to develop in a more defined sequence and may remain for longer periods.
MPOX, previously known as monkeypox, is a viral disease that has garnered significant attention in recent years due to its resurgence and potential impact on public health. This zoonotic infection is primarily transmitted from animals to humans, but it can also spread between individuals through close contact. Symptoms typically include fever, rash, and swollen lymph nodes, which can escalate to more severe complications in some cases. Understanding the transmission, symptoms, and preventive measures is crucial in managing outbreaks effectively. For more detailed information on MPOX, including its epidemiology and clinical features, visit the CDC's official MPOX page.
While most people recover from MPOX without long-term effects, some may experience complications such as skin pigmentation changes or scarring. Severe cases can lead to complications like pneumonia or secondary bacterial infections, particularly in immunocompromised individuals.
Treatment Options for MPOX
Antiviral medications, such as tecovirimat and brincidofovir, have been developed for the treatment of MPOX. These medications have shown effectiveness in reducing the severity and duration of symptoms in clinical settings, although their availability may vary by region.
Supportive care is crucial for those suffering from MPOX, including pain management, maintaining hydration, and managing secondary infections. Patients are advised to rest and avoid contact with others to limit the virus's spread during illness.
In severe cases, hospitalization may be necessary for intensive monitoring and treatment of complications. Emergency treatments may involve advanced care strategies, especially for patients facing respiratory or systemic complications.
Prevention Strategies for MPOX
Vaccination against MPOX has shown promise in providing immunity and preventing outbreaks. The JYNNEOS vaccine, specifically designed to protect against Orthopoxviruses, may be administered to high-risk groups in endemic areas during outbreaks to boost herd immunity.
Safe practices to avoid MPOX transmission include avoiding contact with infected individuals and wild animals, practicing good hygiene, and ensuring that any wounds or cuts are covered. Public education campaigns help raise awareness about transmission routes and preventive measures.
Public health campaigns play a significant role in controlling the spread of MPOX, emphasizing the importance of vaccination, early detection, and timely reporting of cases to authorities. Effective communication strategies can significantly reduce fear and stigma associated with the disease, facilitating better community responses during outbreaks.
MPOX and Public Health
MPOX outbreaks have underscored the need for comprehensive epidemiological surveillance to track infection rates, identify potential zoonotic sources, and understand transmission patterns. Continued monitoring will be essential in managing the ongoing risk of outbreaks globally.
Healthcare providers play a vital role in the management of MPOX through proper diagnosis, reporting, and educating patients about the disease. Developing protocols within healthcare facilities is crucial for preparedness and response to MPOX cases.
The global response to MPOX public health challenges necessitates collaboration among nations to share data, resources, and research findings. International health organizations are pivotal in coordinating responses to reduce the impact of MPOX on public health systems worldwide.
Living with MPOX
For individuals recovering from MPOX, managing daily life involves adhering to medical advice, monitoring for any lingering symptoms, and gradually resuming normal activities. Staying informed about potential complications is also essential.
Support resources for MPOX survivors include counseling services, support groups, and educational materials to help them understand their health status and navigate the recovery process. Connecting with others who have experienced similar challenges can provide emotional support.
Mental health considerations during MPOX recovery are critical, as the stress of illness and the experience of stigmatization can affect an individual's wellbeing. Providing access to mental health resources and fostering open discussions about post-illness emotional challenges can greatly aid recovery.
